Understanding OCD Lesions in the Knee
Osteochondritis dissecans (OCD) of the knee is a joint condition that affects the bone and cartilage, often occurring in children and adolescents. This condition develops when a small segment of bone beneath the cartilage loses its blood supply and begins to separate from the surrounding area. OCD lesions in the knee can cause pain, swelling, and limited joint motion, potentially leading to long-term complications if left untreated.
The exact cause of OCD remains unknown, but factors such as repetitive stress on the joint, low vitamin D levels, and genetic predisposition may contribute to its development. The most common location for OCD in the knee is the lateral aspect of the medial femoral condyle. Diagnosis typically involves radiographic imaging, with MRI often necessary to determine the size and stability of the lesion and assess the degree of cartilage damage.
Treatment options for OCD lesions in the knee vary depending on the severity and stability of the affected area. Non-operative approaches may be suitable for some cases, while others may require surgical intervention to restore joint function and prevent the progression of osteoarthritis. Early detection and appropriate management are crucial for optimizing outcomes and preserving long-term joint health.
Understanding OCD Lesions
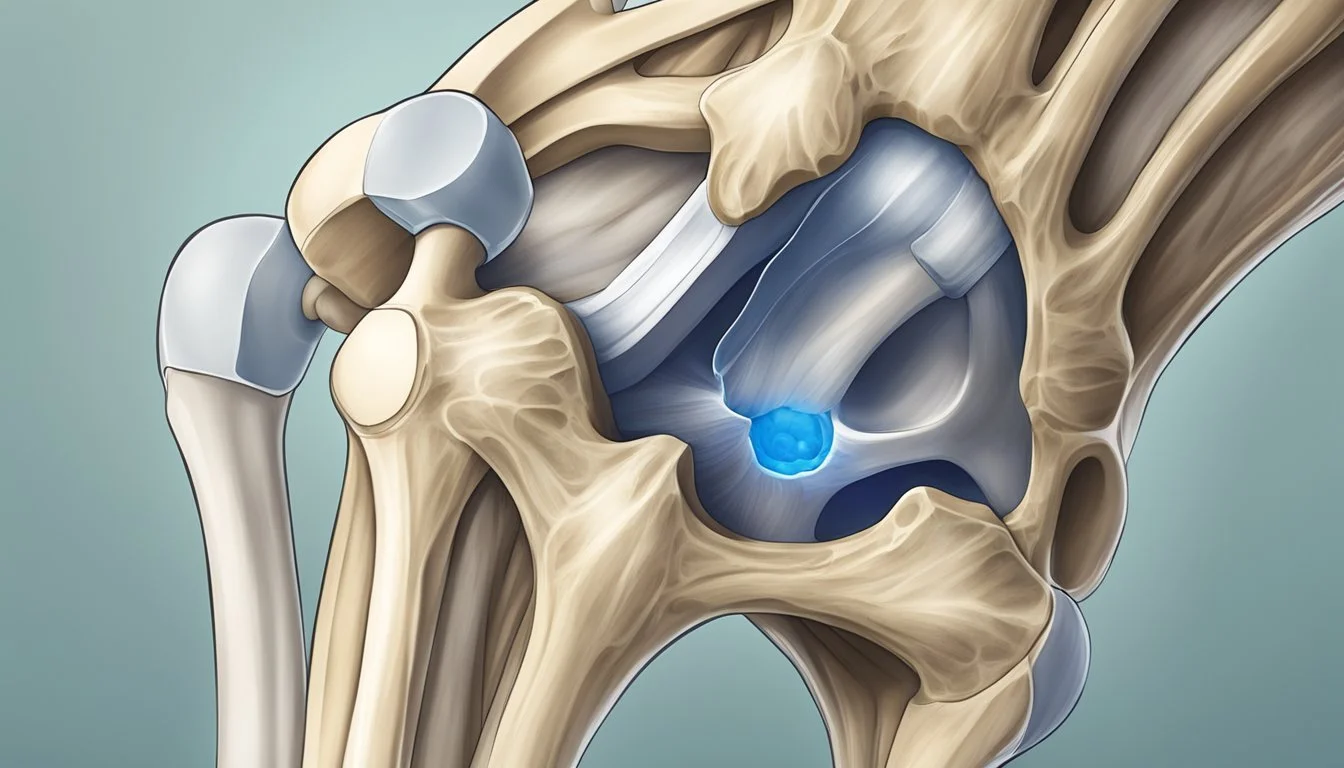
Osteochondritis dissecans (OCD) lesions affect the articular cartilage and subchondral bone in joints, most commonly the knee. These lesions typically occur in the lateral aspect of the medial femoral condyle.
OCD disrupts the normal structure of the joint. The affected area experiences compromised blood supply, leading to weakening of the bone and overlying cartilage.
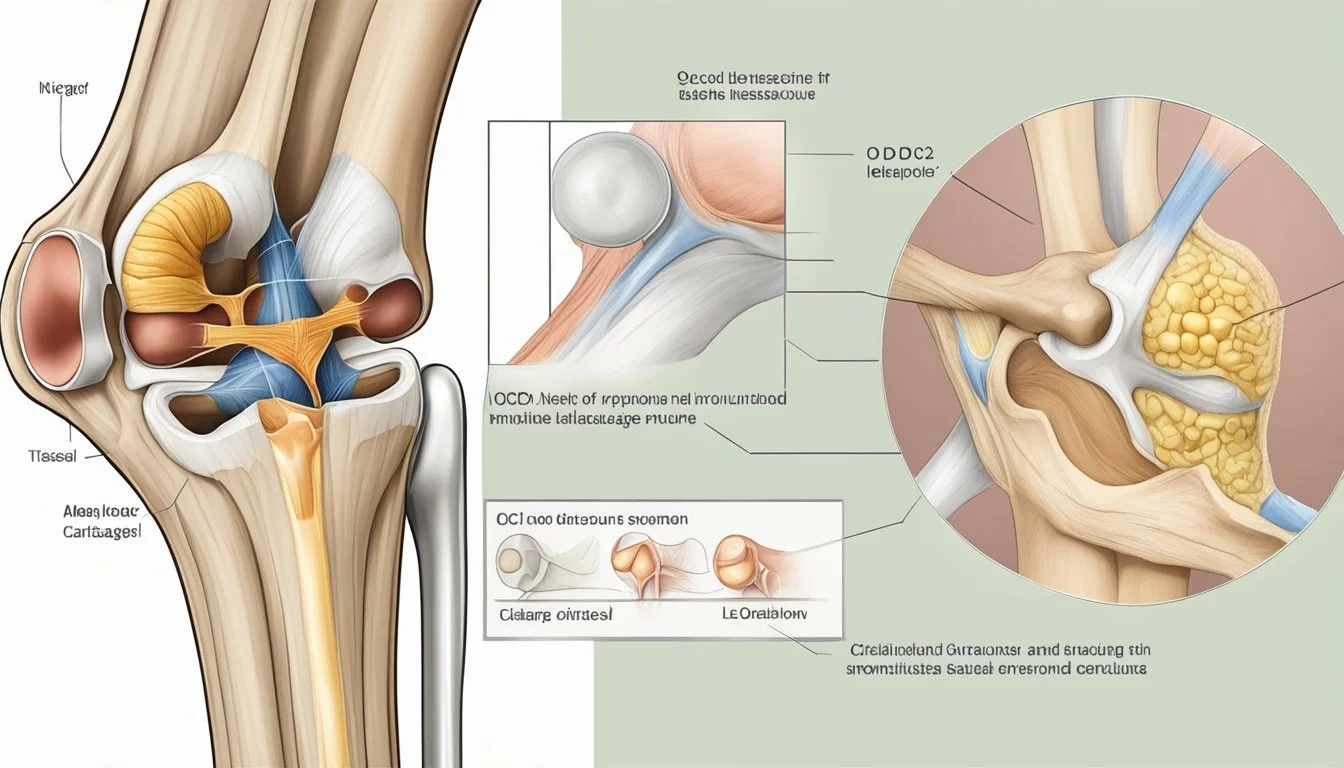
Lesions are classified as stable or unstable:
Stable lesions: Intact articular cartilage
Unstable lesions: Compromised cartilage with potential cracking or separation
The progression of OCD can result in the affected bone and cartilage fragmenting away from the joint surface. This may create loose bodies within the joint space.
Common symptoms include:
Anterior knee pain
Variable joint swelling
Limited range of motion
Diagnosis often involves radiographic imaging, with MRI providing detailed information on lesion size, stability, and cartilage damage extent.
Treatment approaches vary based on lesion stability and patient age. Juvenile OCD generally has a better prognosis compared to adult cases. Conservative management may be suitable for stable lesions, while unstable or advanced cases might require surgical intervention.
Understanding the anatomy of the knee joint is crucial in managing OCD. The condition can affect various structures, including the femur, tibia, and patella, impacting overall joint function and mobility.
Epidemiology and Etiology
Osteochondritis dissecans (OCD) of the knee predominantly affects adolescents and young adults. The incidence ranges from 2.3 to 31.6 cases per 100,000 people, with variations due to ethnicity, sex, and age.
Males are more commonly affected than females, with a ratio of approximately 5:3. The condition typically peaks between ages 13 and 17, rarely presenting before age 6.
The exact cause of OCD remains unclear, but several factors are believed to contribute:
Repetitive microtrauma
Vascular insufficiency
Genetic predisposition
Rapid growth during adolescence
Some studies suggest a hereditary component, as OCD has been observed in multiple family members. However, no specific genetic markers have been definitively identified.
Increased participation in competitive sports and intensive training at young ages may contribute to the rising incidence of OCD. The condition often affects the lateral aspect of the medial femoral condyle, though other knee joint locations can be involved.
Early diagnosis and appropriate management are crucial for optimal outcomes in children and adolescents with OCD lesions of the knee.
Clinical Manifestations
Osteochondritis dissecans (OCD) lesions in the knee present with distinct symptoms and physical examination findings. These manifestations can vary depending on the severity and stage of the condition.
Symptoms Presentation
Pain is the primary symptom of OCD lesions in the knee. It typically worsens with activity and improves with rest. Patients may describe a dull ache or sharp pain, often localized to the affected area of the joint. Swelling can occur, especially after physical exertion.
Mechanical symptoms are common. These include catching, locking, or giving way of the knee. Some patients report a clicking sensation during movement. Stiffness may be present, particularly in the morning or after periods of inactivity.
As the condition progresses, patients might experience decreased range of motion. This can affect daily activities and athletic performance. In severe cases, loose bodies in the joint can cause sudden, intense pain and locking.
Physical Examination Findings
On examination, the affected knee may appear swollen. Palpation often reveals tenderness over the lesion site, typically the medial femoral condyle. Joint effusion might be present, indicating inflammation within the knee.
Range of motion testing may show limitations, especially in flexion and extension. The examiner might feel or hear crepitus during movement. Wilson's test is often positive, eliciting pain when the examiner extends the knee from a flexed position while applying internal rotation.
In advanced cases, loose bodies may be palpable within the joint. The patient might demonstrate an antalgic gait to avoid pain. Quadriceps atrophy can develop over time due to disuse of the affected leg.
Key physical findings:
Joint line tenderness
Effusion
Limited range of motion
Positive Wilson's test
Possible palpable loose bodies
Diagnostic Imaging
Accurate diagnosis of OCD lesions in the knee relies heavily on imaging techniques. These methods help identify the location, size, and stability of the lesion, guiding treatment decisions.
Radiographic Assessment
X-rays serve as the initial imaging modality for suspected OCD lesions. Standard radiographs include anteroposterior (AP), lateral, and tunnel views of the knee. These views can reveal irregularities in the subchondral bone, such as flattening or fragmentation.
The tunnel view is particularly useful for visualizing lesions in the posterior aspect of the femoral condyles. In some cases, loose bodies may be visible within the joint space.
Radiographs also help assess the skeletal maturity of younger patients, which is crucial for determining treatment options.
Advanced Imaging Techniques
Magnetic resonance imaging (MRI) is the gold standard for evaluating OCD lesions. It provides detailed information about the articular cartilage, subchondral bone, and surrounding soft tissues.
MRI can determine lesion stability, a key factor in treatment planning. Unstable lesions may show fluid signal between the fragment and underlying bone.
T2-weighted sequences are valuable for assessing cartilage integrity and detecting joint effusion. MRI also aids in measuring lesion size and depth, which influence prognosis and guide surgical decisions.
In some cases, CT scans may be used to better visualize bony details and fragment position. This can be particularly helpful in preoperative planning for complex lesions.
Treatment Options
Treatment for osteochondritis dissecans (OCD) of the knee aims to promote healing, restore joint function, and prevent long-term complications. The approach depends on the severity of the lesion, patient age, and activity level.
Nonsurgical Management
Nonsurgical treatment is often the first line of approach for stable OCD lesions. Rest and activity modification are crucial to allow the affected area to heal. Immobilization with a cast or brace may be necessary for 4-6 weeks to protect the joint. Limited weight-bearing using crutches helps reduce stress on the knee.
Physical therapy plays a key role in rehabilitation. Exercises focus on maintaining strength and flexibility without aggravating the lesion. Low-impact activities like swimming or cycling may be recommended as alternatives to high-impact sports.
Nonsteroidal anti-inflammatory drugs can help manage pain and swelling. In some cases, doctors may use electrical stimulation to promote bone healing.
Surgical Interventions
Surgery becomes necessary for unstable lesions or when conservative treatment fails. Arthroscopic procedures are common, allowing surgeons to assess and treat the lesion with minimal invasiveness.
Drilling small holes in the lesion (microfracture) stimulates blood flow and healing. For larger defects, surgeons may use osteochondral autograft transfer, taking healthy cartilage and bone from a non-weight-bearing area of the knee.
Fixation techniques, such as bioabsorbable pins or screws, can reattach loose fragments. In severe cases, osteochondral allograft transplantation may be required, using donor tissue to replace the damaged area.
Post-Operative Care
Recovery after OCD surgery typically involves a period of protected weight-bearing, often with crutches. Patients wear a brace to limit knee motion and protect the repair site.
Physical therapy is essential for regaining strength, flexibility, and function. It starts with gentle range-of-motion exercises and progresses to strength training and sport-specific activities.
Full recovery can take 3-6 months or longer, depending on the procedure. Patients must follow their surgeon's guidelines closely to ensure optimal healing. Regular follow-up appointments and imaging studies help monitor progress and guide the return to normal activities.
Surgical Techniques and Considerations
Surgical management of osteochondritis dissecans (OCD) lesions in the knee involves several techniques tailored to the specific characteristics of the lesion. The choice of procedure depends on factors such as lesion size, stability, and location.
For stable lesions, drilling is often employed to stimulate healing. This technique involves creating small channels in the subchondral bone to promote blood flow and repair.
Unstable lesions may require fixation to secure the fragment in place. Surgeons use various methods including:
Bioabsorbable screws
Kirschner wires
Metal screws
Internal fixation aims to promote healing and maintain the integrity of the articular cartilage surface.
For larger defects, grafting procedures are considered. Options include:
Osteochondral autograft transplantation (OATS)
Autologous chondrocyte implantation (ACI)
Osteochondral allograft transplantation
OATS involves harvesting healthy cartilage and bone from a non-weight-bearing area of the knee and transplanting it to the defect site. This technique is particularly useful for smaller lesions.
ACI is a two-stage procedure where cartilage cells are harvested, cultured, and then implanted into the defect. It is often reserved for larger lesions with intact subchondral bone.
Microfracture can be employed for smaller lesions, creating small perforations in the subchondral bone to stimulate fibrocartilage formation.
Prognosis and Outcomes
OCD lesions in the knee generally have a favorable prognosis, especially when diagnosed and treated early. The outcomes largely depend on factors such as lesion size, location, and stability.
For stable lesions treated conservatively, healing rates can reach up to 50-67%. Younger patients with open growth plates tend to have better outcomes due to their higher healing potential.
Surgical interventions for unstable lesions show promising results. Fixation techniques have reported success rates of 80-90% in achieving lesion healing and symptom resolution.
Long-term studies indicate that 60-80% of patients maintain good to excellent knee function after OCD treatment. However, 10-20% may develop osteoarthritis in the affected joint over time.
Recovery timeframes vary:
Conservative treatment: 3-6 months
Surgical intervention: 6-12 months for full return to activities
Factors associated with better outcomes include:
Early diagnosis
Smaller lesion size (<2 cm)
Medial femoral condyle location
Adherence to rehabilitation protocols
Regular follow-up is crucial to monitor healing progress and prevent potential complications. With appropriate management, most patients can expect a return to normal activities and sports participation.
Complications of OCD Lesions
OCD lesions in the knee can lead to several complications if left untreated or if treatment is delayed. The most common issue is persistent pain and discomfort, which may worsen with physical activity.
Joint instability is another potential complication. As the affected bone and cartilage fragment or separate, the knee may feel unstable during movement, increasing the risk of falls or further injury.
Mechanical symptoms like catching, locking, or giving way of the knee can occur. These symptoms result from loose fragments interfering with normal joint mechanics.
In severe cases, OCD lesions may progress to osteoarthritis. The damage to the articular cartilage can accelerate wear and tear within the joint, leading to early-onset degenerative changes.
Avascular necrosis is a serious complication associated with OCD. The lack of blood supply to the affected area can cause bone tissue death, potentially leading to collapse of the joint surface.
Fractures or further fragmentation of the unstable lesion may occur, especially with continued physical activity. This can result in loose bodies within the joint, exacerbating symptoms and causing additional damage.
Growth disturbances are possible in skeletally immature patients with OCD. The lesion may affect the growth plate, potentially leading to limb length discrepancies or angular deformities.
Prevention Strategies
Preventing OCD lesions in the knee involves several key approaches. Proper technique and training are essential for athletes engaged in high-impact sports or activities that stress the knee joint.
Coaches and trainers should focus on teaching correct form and movement patterns to reduce excessive forces on the knee. This includes proper landing techniques, cutting maneuvers, and deceleration strategies.
Adequate rest and recovery between intense physical activities is crucial. Athletes should avoid overtraining and allow sufficient time for their bodies to heal and adapt.
Wearing appropriate protective gear and using proper equipment can help distribute forces more evenly and reduce the risk of trauma to the knee. This includes well-fitting shoes with proper support for the specific sport or activity.
Gradual progression in training intensity and volume helps prevent overuse injuries. Athletes should increase their workload slowly over time rather than making sudden, dramatic changes.
Maintaining overall physical fitness, including strength and flexibility of the muscles surrounding the knee, can provide better joint stability and reduce injury risk.
Regular health check-ups and early intervention for any knee pain or discomfort can help identify and address potential issues before they become more serious.
Lastly, athletes should be educated about the importance of listening to their bodies and reporting any persistent pain or discomfort to medical professionals promptly.
Recent Advances and Research
Significant progress has been made in understanding and treating osteochondritis dissecans (OCD) lesions of the knee. Researchers have developed more sophisticated imaging techniques to assess lesion stability and guide treatment decisions.
Advanced MRI protocols now allow for better visualization of the cartilage-bone interface. This helps surgeons determine whether a lesion is stable or unstable, which is crucial for treatment planning.
Surgical techniques have also evolved. Arthroscopic drilling and fixation methods have become more refined, leading to improved outcomes for many patients.
For juvenile OCD, there's increasing evidence supporting conservative management. Studies show that many young patients with stable lesions can heal without surgery if given adequate time and activity modification.
Tissue engineering approaches are showing promise. Researchers are exploring the use of:
Autologous chondrocyte implantation
Bone marrow stimulation techniques
Growth factor therapies
These methods aim to enhance healing and cartilage regeneration, particularly for larger or more complex lesions.
Biomechanical studies have shed light on the forces acting on different parts of the knee. This knowledge helps in understanding why certain areas are more prone to OCD and informs surgical repair strategies.
Long-term follow-up studies are providing valuable data on the natural history of OCD. This information helps clinicians make more informed decisions about when to intervene surgically versus continuing conservative treatment.